Searching for an explanation about why N.M. pediatric hospitals are overflowing

New Mexico’s hospitals are overrun with sick children.
Numerous medical experts have said over the past couple weeks that part of the reason is that the public health measures New Mexico took in response to COVID made it so children did not get exposed to respiratory viruses as they normally would have.
But in interviews with Source New Mexico, an immunologist and an evolutionary biologist find that explanation to be incomplete, and an explanation could include the fact that COVID attacks the immune system, and like other respiratory viruses, makes a person’s airways more susceptible to infection.
Dr. John Pederson, medical director of the Children’s Program at Presbyterian Healthcare Services, appeared in a joint news conference on Nov. 14 with medical professionals from the other two large hospital systems in New Mexico: Lovelace and the University of New Mexico.
“I think that there is no doubt that the COVID-19 pandemic and the restrictions that we had in place are playing a role,” Dr. Pederson said.
“We are seeing children that typically would have been exposed to these viruses in the past through the annual or seasonal surge that aren’t, and so we do kind of have this immunity gap, this lack of immunity in the community,” he said.
The term “immunity gap” is not identical but strikingly similar to a concept called “immunity debt,” which was invented last year and has faced criticism from some health care workers as flawed conjecture not based on science.
“Adults shouldn’t be having children pay off the debts with viruses that put them in the hospital,” said Anthony Leonardi, an immunologist and public health student at Johns Hopkins University.
If we’re going to use this analogy, then what’s actually going on is “immunity theft,” said Ryan Gregory, an evolutionary biologist at the University of Guelph in Canada.
“COVID is robbing you of a functioning immune system, and so the more times they break in, the less you have in order to make use of to stop these infections,” he said. “So over time, this could become a worse effect. I don’t know if that’s true, but I think it’s a very legitimate possibility, and that’s not something to dismiss, given the stakes.”

On the same day as Dr. Pederson’s comments, New Mexico’s top academic medical center published a news release titled, “Immunity Gap: Susceptibility to Viral Illnesses Driving a Surge in Pediatric Hospitalizations.”
The University of New Mexico Health Sciences Center wrote: “Children staying home during the COVID-19 pandemic likely created an ‘immunity gap’ that is driving a surge of pediatric illnesses that are placing a growing strain on New Mexico hospitals. Many kids who normally would have been exposed to common viruses like RSV and influenza at an early age were isolated from others for up to two years, meaning they never developed immunity to these diseases — and now they are falling ill.”
These two sentences contain five claims based on assumptions and predictions.
These claims need to be tested, and it’s not a given that the idea of an “immunity gap” is the only explanation for the surge in severe cases resulting in hospital admissions we are seeing right now, Gregory said.
Here’s a closer look at what we still need to know in order to fully explain the high number of severe respiratory infections happening in New Mexican children.
1. “Children staying home during the COVID-19 pandemic …”
Children in New Mexico did stay home, but they did not do so from the start of the pandemic up until today.
Schools in 25 New Mexico counties were cleared to begin hybrid learning on Sept. 8, 2020. All New Mexico schools were required to reopen in-person learning on April 5, 2021. New Mexico also lifted its statewide mask mandate in February 2022.
2. “… Likely created an ‘immunity gap’ …”
This is probably trivially true at the level of the entire New Mexico population, Gregory said, but that does not mean children did not exercise their immune systems when they were at home or when masking was in place.
New Mexico’s Acting Health Secretary Dr. David Scrase said during a news conference on Nov. 17 there is no evidence to show any kind of “immunity gap.”
“I don’t think it’s an immune system phenomenon, per se,” Scrase said. But what he thinks happened is we saw a remarkably low incidence of RSV and flu for the past two seasons, he said.
“That’s due to the fact that everyone was masked up for COVID, or even kids not in school, where they’re transmitting, and that is why we saw it,” Scrase said. “So I think what we’re seeing now is what we used to see when people didn’t wear masks all the time.”
Masks, social distancing and handwashing really did work when we were being super careful, said Deputy Health Secretary Dr. Laura Parajon.
“During that time period, we weren’t getting as sick. Kids weren’t getting as sick. And we’re seeing now the impact of not being as careful with our practices,” she said.
So perhaps policymakers should consider cleaning the air in those schools by prioritizing ventilation and filtration, Gregory said, and introduce masks again at the height of these viral seasons.
“I don’t mean shut the schools, but I don’t see how you can have it both ways,” Gregory said. “If those mitigation measures stopped RSV and flu and other things over the last couple years, and children’s hospitals are being completely overrun, we know those mitigation measures will stop that. Why aren’t we stopping it?”

3. “… That is driving a surge of pediatric illnesses …”
This seems to imply there are way more cases than usual. Dr. Anna Duran, associate chief medical officer at UNM Hospital, also said she thinks we are seeing more cases.
But DOH numbers don’t support this theory. Data appear to show New Mexico is experiencing an early surge in respiratory illness, but we have not reached the peaks in two of the previous three winters. We had a really bad year in the winter of 2019-2020, and a pretty bad year above baseline last year.
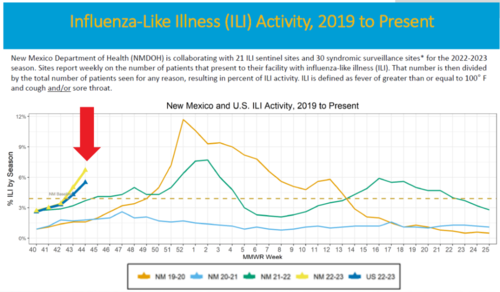
So it is not the case, at least in New Mexico, that mitigations stopped RSV for two years and now we’ve got this huge wave, and that explains why kids are in the hospital.
So why weren’t children’s hospitals in New Mexico and elsewhere in the U.S. overrun in December of 2021? If we’re not necessarily seeing more cases, but the children’s hospitals are overrun right now, what explains that?
4. “… that are placing a growing strain on New Mexico hospitals.”
This is saying the increase in cases is driving the increase in hospitalizations. Does DOH’s data support that explanation?
Hospitalizations increased for COVID by 40%, influenza by 340%, and RSV by 365% over the course of October 2022, according to DOH’s own data.
But DOH doesn’t routinely publish the percentage of people testing positive for RSV and having severe cases, so we don’t know whether the relative number of severe RSV cases has gone up.
This also raises the question: What percent of pediatric RSV cases are resulting in hospital admissions in New Mexico? And how does that stack up to previous years?
No comment
Source New Mexico requested interviews with Dr. Walter Dehority, an expert in pediatric infectious disease and evidence based medicine at the University of New Mexico; and Dr. Miranda Durham, the medical director of the Infectious Disease Bureau at DOH. Neither UNM nor DOH made them available for interviews for this story. We’ll update this story if we hear back.
Another possibility, Gregory said, is that the percentage of those RSV cases that are severe is higher — regardless of whether the number of infections increased.
If that’s true, there’s two explanations: the hosts have changed somehow or the virus has changed somehow, Gregory said.
It could be that all three of those things are true: We have more infections, we’re more susceptible to severe cases, and RSV is worse, he said.

5. “Many kids who normally would have been exposed to common viruses like RSV and influenza at an early age were isolated from others for up to two years.”
Source New Mexico asked Presbyterian for a follow-up interview with Dr. Pederson. They said he was too busy and would not be available until Nov. 28.
Instead, Dr. Pederson sent a written statement which reads, in part, that children being admitted into hospitals are “between 1 and 3-years-old whose immune systems have not seen the routine respiratory viruses that usually circulate each year.”
If the children with respiratory viruses severe enough to be admitted to New Mexico hospitals were not even born two years ago when schools were closed, and are not school-aged right now, then whether those schools were open has nothing to do with why they are getting severely sick right now, Gregory said.
Other possible factors that need to be studied could include whether those children are being infected at daycares or by their school-aged siblings, who could be bringing respiratory infections home from school, Gregory said.
What else could explain what’s happening?
What Pederson and UNM Hospital officials are saying is plausible and must be true to an extent, Gregory said, but it also shuts down discussion about anything else.
There is a pretty good alternative hypothesis that is deeply concerning to Gregory: Infection with COVID can impede immune function, and a higher percentage of children are susceptible to a severe infection.
Leonardi, the immunologist, studies T cells, one of two kinds of white blood cells that defend the body against infection.
Here’s how it works:
T cells get stimulation from the small pieces of protein found in a virus called antigens.
COVID strongly stimulates T cells and corrupts them so they start attacking the body by infiltrating organs and killing cells, Leonardi said.
Another immune system cell at play is called plasmacytoid dendritic cells. They help T cells by presenting them with the antigens.
Dendritic cells also help control viruses before infection by producing interferon alpha, which can be the difference between a severe and a mild case of RSV, Leonardi said.
These dendritic cells, seven months after a mild COVID infection, were “wiped out” in adults, Leonardi said.
“The entire cohort of adults with mild COVID infection, they have those plasmacytoid dendritic cells very low, almost wiped out, compared to somebody who didn’t have a COVID infection,” Leonardi said. “And after seven months, the numbers weren’t back up. They were flat.”
Leonardi suspects that is the same effect in children, because COVID could be lowering the amount of these helper cells in their bodies.
And other research has shown that every time you get infected with COVID, you are accumulating more organ damage.
It is possible COVID is playing some part in the severity and number of children who are catching RSV and flu, Leonardi said.
We shouldn’t dismiss the very significant possibility that COVID infection is making some subset of people who already had the illness more susceptible to severe infection, Gregory said.
“Let’s say you double or triple the number of people who get severe infection because they had COVID. That’s enough to overwhelm pediatric hospitals, which normally are already pretty close to capacity,” Gregory said. “So it’s a big deal to get it correct.”









