Avera receives $2.5 million in federal money for rural nurse shortage

South Dakota-based Avera Health recently received over $2.5 million to address nursing and health care workforce shortages in rural South Dakota through virtual nursing and education.
The funding comes from the Health Resources and Services Administration, an agency of the U.S. Department of Health and Human Services.
South Dakota’s nursing shortage is years in the making, but was accelerated by the COVID-19 pandemic. Many nurses chose to leave the profession or retired early because of the influx of patients and increased stress.
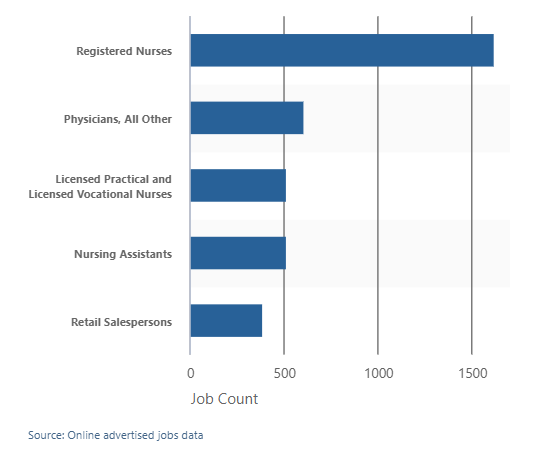
Registered nursing is the most in-demand South Dakota occupation advertised online as of mid-November on the South Dakota Department of Labor and Regulation job board. There are about 1,000 more job postings for the occupation than the second most-common posting: physicians. Nursing assistants and licensed practical and vocational nurses closely follow in third and fourth.
The pipeline for attracting more people to the nursing field, especially in rural areas, is tapped out. Health care systems like Avera are turning to alternative solutions including educational partnerships, virtual health care and nursing support — all of which is covered through the recent funding.
Outside of the grant funding, Avera recently implemented an internal travel nursing program to address nursing recruitment and retention. The health care system will also soon hire nurses internationally.
Rural areas and critical access hospitals are South Dakota’s “most acute health workforce need,” said Karna Pfeffer, director of clinical excellence and education at Avera St. Mary’s Hospital in Pierre.
“The more rural facilities feel it a lot harder and faster when they lose one nurse,” Pfeffer said. “At a larger facility you can absorb that loss and can pick up that shift. But when your pool of nurses is six wide, that one loss is a significant portion of your workforce.”
Virtual care supports rural nurses, won’t replace them
The first grant covered in the federal funding is Project NEXT, a $1.5 million grant to support a three-year training program for rural health professionals on how to use telehealth and health information technology.
Cross-training professionals in virtual nursing will allow rural nurses to handle in-person patient care while virtual nurses will help with documentation and offer support.

“(Virtual care) isn’t going to replace rural care. It’s not ever going to replace rural nurses,” Pfeffer said. “As a new grad coming into a facility, sometimes you’re only one nurse on the floor for a 12-hour night shift. Having the ability and support of another nurse virtually will hopefully reduce anxieties that a new grad nurse will have and allow them to start their practice at a rural facility more confidently.”
The move to virtual care is exploring what the “right path” is for health care after the COVID pandemic. Health care systems are choosing to look at what patients need, the delivery of care, and how to give care as close to the patient’s home as possible.
“Project NEXT offers Avera an opportunity to support nursing staff, not simply by hiring more RNs, but also by leveraging the capacity of its health IT workforce to intervene in ways that are new and cutting-edge,” said Rachael Sherard, senior vice president for rural health at Avera, in a news release.
South Dakota was a priority state for the NEXT grant due to low projection of available nurses compared to surrounding states.
University partnerships to make future nurses more comfortable with rural care
Thirty percent of new RN graduates at South Dakota universities leave the state after graduation.
It’s imperative to find ways to retain those recent graduates in South Dakota, Pfeffer said.

“We all know if you go somewhere and get comfortable with your job, then you stay,” she said. “If we can make these future nurses comfortable with (rural health care) while in nursing school, then they’ll choose to work at critical access hospitals and possibly stay there for the next 15 years.”
The second grant, part of the Nurse Education, Practice, Quality and Retention Registered Nurse Training Program, provides $1 million in funding over three years. The project will partner with South Dakota State University’s nursing program to prepare future nurses for careers in rural acute-care critical access hospitals.
The grant provides education in cultural awareness, social determinants of health, health equity and health literacy. The grant aims to remove barriers and perceptions about practicing in a rural acute-care setting.
Avera Health will also expand its training for college nurse clinicals and precursors to rural settings and practice outside of Sioux Falls, which will expose them to work in rural hospitals. Urban hospital care is significantly different from rural nursing, Pfeffer said.
“In more urban areas there are more resources for students to divert patients to, whereas in smaller areas it comes down to nurses to understand and find solutions to those problems,” Pfeffer said. “Getting a better understanding and awareness of that difference will set them up for success.”








